When you hear the words “voice therapy”, you may imagine this primarily targets professional voice users (e.g., people who rely on their voice for their jobs) or individuals with extensive medical diagnoses. However, voice therapy can spread far beyond these demographics and can possibly help your child! Pediatric voice therapy is not often discussed as its area of impact is not as pervasive as articulation or language disorders. Follow along here to learn more about what pediatric voice therapy is and how it can help your child.

What is pediatric voice therapy? Why should I consider this for my child?
Voice therapy supports using one’s voice at its optimum function. This means that all the muscles involved with making the voice work are trained to coordinate with one another to allow for the appropriate amount of tension and movement function. Additionally, voice therapy targets respiratory support in order to give the voice the appropriate amount of “fuel” to sound healthy and clear.
If your child is struggling with their voice production, it is likely they are already aware of it. Children as young as 6 are aware of differences in their voice, which may make them hesitant to participate in vocal activities. These activities can include singing, acting, yelling in sports, participating in class, or talking with peers. Studies show that persistent voice disorders impact children’s participation in hobbies as well as overall quality of life. It is true that in many cases, children eventually grow out of their voice disorder. However, its impact may outlast the disorder itself.
Signs that your child may benefit from voice therapy:
Voice therapy targets muscle coordination and respiratory support to allow for optimal voice production while reducing vocal behaviors that may cause damage to the vocal folds. Considering this, here are some signs that your child may benefit from voice therapy:
- Hoarseness or roughness
- Breathiness or weakness
- Report of feeling fatigued after talking
- Sensation of a lump in the throat
- Inappropriate pitch range for age level
- Delayed voice initiation (e.g., breathiness or silence at the start of trying to talk, followed by a hard onset)
- Frequent throat clearing
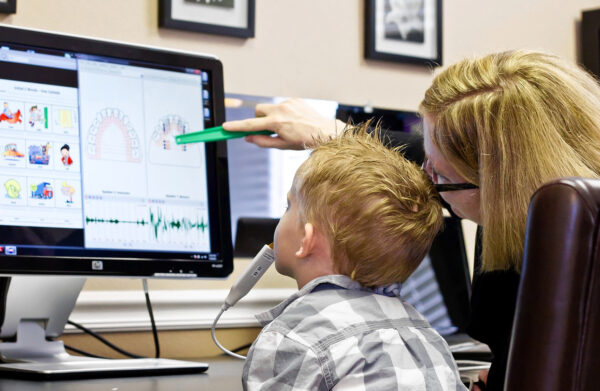
What happens in voice therapy?
Depending on your child’s diagnosis, voice therapy sessions typically extend from 6-8 sessions with one session per week. In these sessions, a variety of muscle relaxation stretches, muscle coordination activities, and breathing exercises take place. These activities might include straw bubbles, humming, silly voice games, and lip trills. For younger children, a more indirect approach is taken to model appropriate voice behavior while working with parent and child to decrease any vocal behaviors that might aggravate the vocal folds.
Counseling can also be provided for healthy vocal hygiene (e.g., proper voice care like drinking enough water, monitoring loudness, taking vocal rest, etc.) to encourage upkeep of their new skillset. The goal of therapy is to eliminate the root cause of the vocal disorder and to give your child the strategies to continue use of a healthy voice.
How can I get my child evaluated?
If you have concerns with your child’s voice, consult with your pediatrician to have imaging done for a full evaluation. It is necessary to assess the child’s vocal folds directly with imaging tools to note any abnormalities. These abnormalities can include nodules or cysts that appear as small bumps on the vocal folds. There may also be improper closure of the vocal folds which would create an abnormal production of voice. Depending on your child’s age, imaging will take the form of laryngoscopy (a camera that extends down one’s tongue or through the nasal cavity) so the assessor can view the folds in their entirety.
In some cases, medical intervention, such as surgical removal, is necessary to repair the abnormality. In these cases, voice therapy is often recommended to educate the patient on appropriate vocal function before medical intervention.
For more information and resources for evaluation, please contact our team today.
Written by Mary Nevins, M.S. CCC-SLP